DOI: 10.20986/resed.2020.3803/2020
ORIGINAL
Identification of signs and symptoms for the diagnosis of discogenic low back pain: mapping review
Identificación de signos y síntomas para el diagnóstico del dolor discal: revisión de mapeo
S. Henao Romero1, J. C. Acevedo González1, L. E. Basto Aluja1and I. S. Moreno Luna2
1Unidad de Neurocirugía, Hospital Universitario San Ignacio. Facultad de Medicina, Pontificia Universidad Javeriana. Bogotá, Colombia
2Departamento de Epidemiología, Pontificia Universidad Javeriana. Bogotá, Colombia
Henao Romero S, Acevedo González JC, Basto Aluja LE, Moreno Luna IS. Identification of signs and symptoms for the diagnosis of discogenic low back pain: mapping review. Rev Soc Esp Dolor. 2020;27(5):1-0
Received: 24-03-2020
Accepted: 07-09-2020
Correspondence: Sara Henao Romero
sarahenaor@gmail.com
ABSTRACT
Objective: Low back pain is one of the most common pathologies in adult population. Its economic burden to the health system and its impact on quality of life and function, makes it a relevant theme. In most of the cases the etiology of pain can be delimitated but a diagnostic scale for discogenic low back pain (DLBP) is not available. Reviewing the most frequent signs and symptoms of DLBP in literature may improve the approach to the patient with pain. Additionally, it may aid the creation of a pilot diagnostic scale for DLBP.
Materials and methods: A systematic review of literature was done over the last 20 years in MEDLINE and BIREME. A mapping review of the most frequent symptoms and signs (clinical and imaging) used to suspect DLBP was conducted. A total of 1010 articles were reviewed, 103 of which were selected to analyze the frequency of reporting signs and symptoms included in the diagnosis.
Results: In the mapping review, the most frequent symptom was axial low back pain, followed by the absence of radicular pain. A lower frequency of description was observed in the literature regarding the signs associated with disc pain, finding mention only in 12 % of the articles of biphasic movements when passing from sitting to standing. The centralization of pain to the physical examination, a positive vibration test and the absence of improvement with facet and sacroiliac infiltration, were other signs found in the review. As for the diagnostic images, the Pfirrmann scale had the highest frequency of appearance, followed by the HIZ (High intensity zone) and Modic changes.
Conclusions: Low back pain is a complex pathology in its treatment and its consequences in the lives of patients. Diagnosing DLD can improve how we manage patients. Symptoms and clinical and radiological signs have a greater diagnostic impact when used together. The characteristics with the highest frequency of appearance in the literature were selected to generate a pilot scale, which should be compared to the gold standard in DLD, discography.
Key words: Intervertebral disc, low back pain, discogenic pain.
RESUMEN
Objetivo: El dolor lumbar constituye una de las patologías con mayor prevalencia en la población adulta. Su carga económica para el servicio de salud e impacto en la calidad de vida y funcionalidad de los pacientes lo convierte en un tema de suma relevancia. En la mayoría de los casos es posible atribuir el dolor a una de las estructuras de la columna lumbar; sin embargo, no existe una escala diagnóstica que permita diferenciar el dolor lumbar de origen discogénico (DLD). La revisión de los signos y síntomas del DLD más frecuentes en la literatura permite un mejor abordaje al paciente con dolor lumbar, y a la vez una aproximación a la creación de una escala diagnóstica piloto para definir DLD.
Materiales y métodos: Se realizó una búsqueda sistemática de la literatura de los últimos 20 años en MEDLINE y BIREME, a partir de la cual se realizó una revisión de mapeo del reporte de los signos y síntomas comúnmente utilizados para sospechar DLD. Se revisaron un total de 1010 artículos, de los cuales se seleccionaron 103 para analizar la frecuencia de reporte de signos y síntomas incluidos en el diagnóstico.
Resultados: En la revisión de mapeo el síntoma más frecuente fue el dolor lumbar axial, seguido por la ausencia de dolor radicular. Se observó menor frecuencia de descripción en la literatura en torno a los signos asociados al dolor discal, encontrando mención solamente en el 12 % de los artículos de movimientos bifásicos al pasar de sedestación a bipedestación. La centralización del dolor al examen físico, el test de vibración y la ausencia de mejoría con bloqueo facetario y sacroiliaco fueron otros de los signos encontrados en la revisión. En cuanto a las imágenes diagnósticas, la escala de Pfirrmann tuvo la mayor frecuencia de aparición, seguida de los cambios HIZ (High intensity zone) y Modic.
Conclusión: El dolor lumbar es una patología compleja en su tratamiento y en sus consecuencias en la vida de los pacientes. El diagnóstico del DLD puede mejorar el enfoque del paciente. Los síntomas y signos clínicos y radiológicos tienen mayor impacto diagnóstico cuando se usan en conjunto. Se seleccionaron las características con mayor frecuencia de aparición en la literatura para generar una escala piloto, que debe ser comparada con el patrón de oro en DLD, la discografía.
Palabras clave: Disco intervertebral, dolor lumbar, dolor discogénico.
INTRODUCTION
The prevalence of low back pain makes it an extremely important issue, considering that 60-80% of adults will be affected by it at some point in their lives (1). As the population pyramid is reversed, this condition becomes more relevant because of the economic burden it generates on the health system, due to the high frequency of emergency consultation the use of resources for its treatment and its impact on the functionality of individuals (1). Low back pain is among the ten diseases generating the highest number of disability-adjusted life years (DALYs), according to the WHO Global Burden of Disease Study in 2010 (2). There are multiple risk factors for the onset of low back pain, including occupational exposures (sedentary lifestyle, lifting of loads), stress and obesity (3). However, the cause of the pain remains hidden in many of the patients.
Low back pain is a complex disease, in which the identification of the structure causing pain is crucial. In most cases, pain can be attributed to one of the lumbar spine structures. Despite the clinical and radiological differences among the different etiologies of low back pain, there is no diagnostic scale that differentiates the discogenic origin of pain. Diagnostic errors lead to therapeutic failures that result in an inappropriate use of resources and an increase in patients’ morbidity. To understand the etiology of discogenic lumbar pain (DLP), it is important to be aware of the elements of the anatomy of the disc and its degeneration.
The intervertebral discs form a biomechanical system with the facet joints providing mobility to the segments. The nucleus gelatinosus absorbs loads due to its viscoelastic properties, and redistributes them radially to the fibrous ring through hydrostatic forces. The alternating laminar structure of the fibrous ring is designed to withstand tensile strength (4). After birth, the vascular contribution decreases, leading to changes in tissue from the second decade of life (5). The percentage of added proteoglycans decreases by proteolytic degradation, and chondroitin sulfate chains are replaced by keratin sulfate chains, due to low oxygen pressure; these changes lead to a decrease in the hydrophilic characteristics of the nucleus and increase the rigidity of the extracellular matrix. This alters the ability to dissipate loads with a thinning of the nucleus, causes the fibrous ring to be directly exposed to axial loads (6).
Disc degeneration can lead to pain conditions secondary to disc herniation, which generates nerve root compression, deformity, and stenosis. However, the disc itself can be the source of lower back pain through its intrinsic innervation (7). In normal adults, the outer third of the fibrous ring is innervated by branches of the sinuvertebral nerve of Luschka and sympathetic branches. During the process of disc degeneration, a neoinnervation has been found associated with the formation of granulation tissue, reaching the inner layers of the fibrous ring, and even to the nucleus gelatinosus (8), and thus contributing to the etiology of DLP.
Radiological changes secondary to disc degeneration are evident in magnetic resonance imaging, with loss of disc height, a decreased T2 signal secondary to lower water content, changes in endplates, and annular tear (5). It is important to understand that intervertebral disc degeneration is not always accompanied by low back pain. However, when this is the etiology of pain, it is characterized by predominating in the middle line, exacerbating with axial loads, sitting position and flexion of the trunk, and not associated with radicular symptoms or alterations in the neurological examination (9).
There is no gold standard for diagnosis of DLP. At present, the reference examination is discogram, it continues being a controversial diagnostic method because of being invasive, having the potential to generate injury at the disc level, a high false-positive rate and low specificity (10). The search for diagnostic methods for a better approach to patients with DLP continues, and it is of great importance for the characterization of patients and the determination of their treatment. In the present study, a literature mapping review was performed on clinical and radiological signs and symptoms allowing the differentiation of pain of discogenic origin from other etiologies of lumbar pain in the adult population.
Materials and methods
A systematic search of the literature published in the last 20 years was performed in MEDLINE and BIREME using the following search terms:
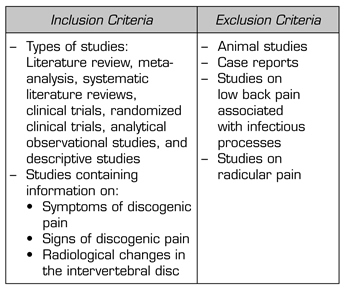
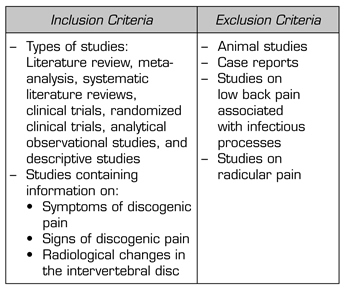
A mapping review of the DLP-associated signs, symptoms, and radiological changes report was performed, taking into account that the search is not about the outcome of an intervention, but about the frequency of the reporting of signs and symptoms. The mapping review allows the identification of the diagnostic criteria presented by the medical literature, without seeking to determine the accuracy of the criteria (Table I).
TABLE I. INCLUSION AND EXCLUSION CRITERIA
A total of 1010 articles were reviewed, and after eliminating duplicates, 103 articles were selected for analysis. The criteria used to determine the diagnostic likelihood of discogenic pain were evaluated for each article. The mapping review does not seek to assess the quality of the articles used, but to evaluate the frequency of reporting the different clinical and radiological signs and symptoms used in the diagnosis of discogenic lumbar pain (Figure 1).
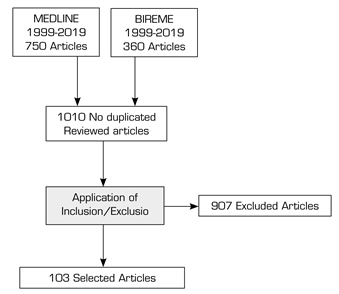
FIGURE 1. SELECTION OF STUDIES
RESULTS
A total of 103 articles describing the criteria used to diagnose the patient with DLP were selected for the mapping review. These criteria were broken down into symptoms, signs and radiological changes in nuclear magnetic resonance imaging.
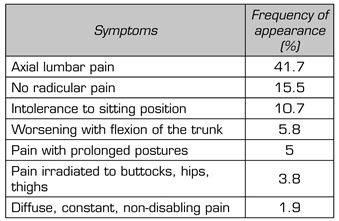
A total of 48% of the 103 studies used symptomatic pain characteristics to identify patients with disc etiology. The frequency of occurrence of these is shown in Table II. The axial location of pain is the most frequent feature, followed by the absence of radicular symptoms. Patients with discogenic pain show exacerbation of symptoms with sitting position, prolonged postures, and trunk flexion. Irradiation to the hips and thighs may accompany axial pain, however this pain has no radicular characteristics. The type of pain (diffuse, constant, non-disabling) does not appear frequently in the literature review.
TABLE II. FREQUENCY OF APPEARANCE OF SYMPTOMS OF DISCOGENIC LUMBAR PAIN
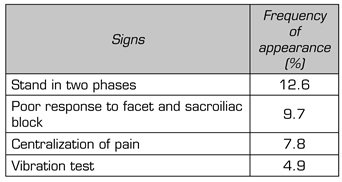
As for signs of physical examination, the difficulty of switching from sitting to standing position, performing this movement in a biphasic movement, was the most frequent sign of appearance in our search. Ten of the analyzed articles ruled out other causes of low back pain by percutaneous management before defining the disc etiology. The phenomenon of centralization of pain during mobilization to physical examination was reported in 8 articles as criterion of discogenic pain. Five studies used pain replication with the vibration test on the neural spines, where by using a device to conduct this sensitive modality (for example, diapason), painful phenomena similar to those usually referred by the patient with DLP can be triggered (Table III).
TABLE III. FREQUENCY OF SIGNS APPEARING ON PHYSICAL EXAMINATION
Nuclear magnetic resonance imaging is an important diagnostic tool in the study of low back pain. Secondary changes to degenerative disc disease can be classified according to their signal using the Pfirrmann scale. This scale assesses the signal intensity of the nucleus gelatinosus in the T2 sequence on magnetic resonance imaging and associates it with the disc degeneration process by scoring the degree of compromise of this structure from one to five points. Within the alterations in nuclear magnetic resonance, the Pfirrmann scale had the highest frequency of appearance as a diagnostic method, as shown in Table IV, finding its largest relevance with score equal to or greater than 2. The appearance of high-intensity signal zones at the back of the fibrous ring in the T2 sequence (High intensity zone - HIZ) has been correlated with the disc etiology of low back pain, and it was found in 27 of the reviewed studies. This phenomenon represents the neovascularization occurring in the posterior annular fissures, as a result of the inflammatory process associated with disc degeneration.
TABLE IV. FREQUENCY OF APPEARANCE OF CHANGES IN NUCLEAR MAGNETIC RESONANCE IMAGING
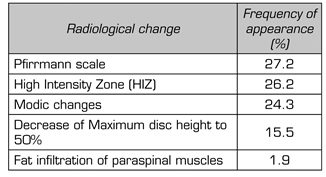
Modic changes are identifiable radiological phenomena in the magnetic resonance imaging at the bone marrow level and at the terminal cartilaginous dishes. Depending on the signal intensity of these structures in the T1 and T2 sequences, three different types of changes are described (Type I: edema, Type II: fatty, Type III: sclerotic). These Modic changes are correlated with the degenerative process of the spine and are associated with a structural compromise impacting on normal physiology, contributing to the presence of instability. Within our review, the Modic changes were found in 25 articles. The decrease in the height of the intervertebral disc was found in 16 studies as part of the diagnosis of discogenic pain, always specifying that the disc should maintain at least 50 % of its original height. Fat infiltration in the paraspinal muscles was found at a low frequency within the review.
DISCUSSION
Intervertebral disc degeneration is a process associated with aging that occurs in both healthy subjects and patients with low back pain (11). Non-herniated disc disease constitutes discogenic pain, which is a diagnosis of exclusion within lumbar conditions (12), so it is common to perform diagnostic tests for other etiologies before determining the intervertebral disc as a source of pain. The diagnosis of disc pain has been based on the discogram with the reproduction of the pain by injecting contrast medium into the intervertebral disc, showing abnormal distribution of the contrast and the presence of one or two adjacent pain-free control discs (7). Its use with adequate technique is a useful method, however, it has been associated with acceleration of degenerative changes in the intervertebral disc (13).
The search for different diagnostic methods for discogenic lumbar pain is essential. The characteristics of low back pain are a fundamental part of the patient’s medical record, and focus the clinician on the diagnosis. The axial location of pain was the most frequent characteristic in our search. However, multiple etiologies can cause pain of these characteristics (14), so it alone is not sufficient diagnostic criteria. In the approach of the patient with low back pain, differentiation between axial or radicular pain is a fundamental step, which explains that the absence of radicular pain is the second most frequent criterion in the determination of symptoms. The pattern of disc pain can be diffuse and irradiated to the region of buttocks, hips and thighs, without a radicular pattern. This distribution is common in other etiologies of low back pain, especially secondary to alterations in the sacroiliac joints (15), and its frequency of appearance in the revised symptoms was low.
The role of the disc in the absorption of the axial load is impaired with its degeneration (6), in addition in in vitro studies has shown that inflammatory changes at the level of the degenerated disc generate secretion of neurotrophic factors, which leads to neoinnervation, important in the pathophysiology of disc pain (16). Secondary to this, discogenic pain is exacerbated by movements that increase pressure on the disc; of these, intolerance to sitting position was the most frequent, followed by pain with the flexion of the trunk and the maintenance of prolonged postures. Seven of the articles describe this as a set of symptoms.
Regarding physical examination, the transition from sitting to standing position in a biphasic way was a common feature of the revised articles. The phenomenon of centralization refers to the movement of pain to the middle line during the performance of exercises of flexion and extension of the spine in decubitus and standing position, and it was described by McKenzie as a suggestive sign of low back pain of disc origin in 1981 (17). The positivity of the vibration test at the disc level, a test that was introduced by Yrjama and Vanharanta in 1994, was found less frequently, showing good correlation with discogram (18).
Radiological alterations are an important part of the identification of the structure responsible for low back pain, however, they can also be found in asymptomatic subjects. The decrease in signal intensity in the T2 sequence is secondary to dehydration and degradation of the nucleus matrix (5), and this is the most frequently reported change in our search. According to its severity, it is classified with the Pfirrmann scale, finding greater clinical relevance with scores equal to or greater than two. HIZ was the second most frequent radiological factor in literature search. It has been suggested that this occurs due to inflammation of the fibrous ring, and that this inflammation irritates the nerve terminals, associating its appearance with the presence of pain (18).
The articular saucers suffer from loss of their vasculature during childhood, resulting in cartilage disorganization and cracks, with subsequent microcracks of the subchondral bone and sclerosis of the endplate (19). In 1998, Modic et al. described changes in signal intensity in nuclear magnetic resonance at the vertebral saucer level, delimiting three phases in the degenerative process: An inflammatory phase, a fat phase, and a sclerotic phase (20). The Modic changes were frequent in the review, followed by the decrease in the height of the disc, preserving at least 50 % of its original size, in order to differentiate it from the herniated or protruded disc. Fat infiltration is a common finding in the lumbar disease of different etiologies, with low frequency of appearance in our review associating it with discogenic pain.
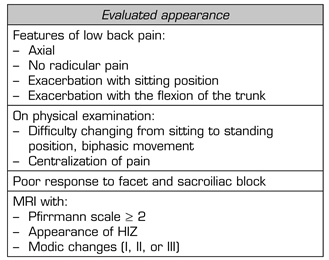
As this is a mapping review, no predictive values for the different characteristics can be determined. However, a pilot diagnostic scale can be generated using the frequency of appearance in the literature of the different symptoms and signs. Table V shows the pilot scale, which must be verified in subsequent studies, comparing its effectiveness with that of the gold standard, in this case, discogram.
TABLE V. PILOT DIAGNOSTIC SCALE BASED ON THE FREQUENCY OF THE APPEARANCE OF SIGNS AND SYMPTOMS IN THE LITERATURE
CONCLUSION
Low back pain is a challenge in clinical practice because of its multifactorial etiology and its impact on patients’ quality of life. When considering the complexity of discogenic lumbar pain, it is important to emphasize that none of these different clinical and radiological symptoms and signs can be used separately for diagnosis. The criteria with the highest frequency of appearance should be understood as a whole, since the highest probability of diagnosis is the result of the sum of all of them. Additional studies are needed to test the pilot scale to determine its effectiveness in diagnosing this type of lower back pain.
CONFLICT OF INTEREST
The authors of the present study have no conflict of interest to declare.
REFERENCES