DOI: 10.20986/resed.2020.3777/2019
ORIGINAL
Spinal cord stimulation. Analysis of diagnostic indications
Neuroestimulación medular. Análisis de las indicaciones diagnósticas
P. Kot1
C. Pintado1
P. Rodríguez1
G. Fabregat1
V. Villanueva1
J. Asensio1
B. Cano2
J. de Andrés3
1Departamento de Anestesia, Reanimación y Tratamiento del Dolor, Consorcio Hospital General Universitario. Valencia, Spain
2Departamento de Enfermería, Hospital Universitario y Politécnico La Fe. Valencia, Spain
3Unidad de Anestesia. Departamento de Cirugía. Facultad de Medicina. Universidad de Valencia, Spain
ABSTRACT
Introduction: Spinal cord stimulation (SCS) is a form of chronic pain treatment that has been shown to be effective in patients who have responded poorly to other therapies. The current indications for SCS devices are very varied. The aim of our study is to analyze the diagnostic indications of SCS therapy during the last 5 years in our hospital, to know the most frequent causes of pain for the indication of the implant of the device and what percentage of improvement patients present, as well as to study the relationship with gender and age.
Material and methods: This is an observational, descriptive, retrospective study. The patients were identified from the surgical activity register of the Pain Unit of the General Hospital of Valencia.
Results: The final number of patients included was 179. The Failed back surgery syndrome (FBSS) was the diagnostic indication in 112 patients (62.57 %). The mean percentage of improvement described by the patients after the SCS implant was 47.99 ± 27.3 %. There were no differences in the improvement with respect to age or gender.
Discussion: In spite of the variability of diagnoses in which this therapy may be indicated, it is noteworthy that in more than half of the cases the indication is by FBSS.
Key words: Spinal cord stimulation, failed back surgery syndrome, chronic pain, neuromodulation
RESUMEN
Introducción: La neuroestimulación medular (NM) es una forma de tratamiento del dolor crónico que ha demostrado su efectividad en pacientes que han respondido mal a otras terapias. Las indicaciones actuales para los dispositivos de NM son muy variadas. El objetivo de nuestro estudio es analizar las indicaciones diagnósticas de la terapia con NM durante los últimos 5 años en nuestro hospital, conocer cuáles son las causas de dolor más frecuentes para la indicación del implante del dispositivo y qué porcentaje de mejoría presentan los pacientes, así como estudiar la relación con el género y la edad.
Material y métodos: Se trata de un estudio observacional, descriptivo y retrospectivo. Los pacientes fueron identificados desde el registro de actividad quirúrgica de la Unidad del Dolor del Hospital General de Valencia.
Resultados: El número final de pacientes incluidos fue de 179. El síndrome de cirugía fallida de espalda (SCFE) fue la indicación diagnóstica en 112 pacientes (62,57 %). La media del porcentaje de mejoría descrita por los pacientes tras el implante del NM fue de 47,99 ± 27,3 %. No se observaron diferencias en la mejoría respecto a la edad o el género.
Discusión: A pesar de la variabilidad de diagnósticos en los que puede estar indicada esta terapia, es destacable que en más de la mitad de los casos la indicación es por SCFE.
Palabras clave: Neuroestimulación medular, síndrome de cirugía fallida de espalda, dolor crónico, neuromodulación
Correspondence: Pablo Kot MD
pablo_kot@hotmail.com
Received: 04-11-2019
Accepted: 07-07-2020
INTRODUCTION
Chronic pain affects about 30% of the population in developed countries (1). Spinal cord stimulation (SCS) is a form of chronic pain treatment that has been shown to be effective in patients who have responded poorly to other therapies. The SCS consists of the implantation of one or more epidural electrodes in the posterior columns of the spinal cord at the level of the dermatomes where the analgesic effect is desired (2).
In 1959, neurosurgeon Willem Noordenbos reported that the signal transmitted along thick fibers for touch, pressure and vibration could inhibit the pain signal transmitted by thinner fibers (3). In 1965 when Melzack and Wall introduced the classical gate-control theory. They proposed that painful stimuli are transmitted to the second neuron of the pain pathway in the posterior horn of the spinal cord, where multiple peripheral neurons converge to a single neuron. According to his theory, the stimulation of Ab fibers, myelinated and non-nociceptive, inhibit the transmission of pain by the Ad and C fibers (4).
The development of spinal cord stimulation devices was one of the consequences of the introduction of the gate theory. Taking their first steps in 1967 with the implantation of electrodes for the first time in a human patient by Shealy et al. (4). The first fully implantable device was developed in 1970 and the first clinical trials on patients with intractable chronic pain were conducted in the early 70s (3). The devices have evolved over the years, with a variety of systems available today, including monopolar, bipolar, cylindrical electrodes, as well as conventional stimulation therapies, high frequency or bursts, among others (5,6). Although the greatest evidence refers to conventional therapy, more and more studies are aimed at providing evidence for new modes of therapy to be able to discern the best indications in each case. Fifty years have passed since the implantation of the first neurostimulator, with more than 50,000 neurostimulators implanted each year in the world today (7).
The current indications for SCS devices are very varied. The International Neuromodulation Society (INS) establishes recommendations (6) in which SCS therapy may be indicated in common chronic pain including: 1) axial pain due to failed back surgery syndrome or radicular pain; 2) neuropathic pain including diabetic neuropathy, HIV neuropathy, complex regional pain syndrome (CRPS), postherpetic neuralgia, intercostal neuralgia, phantom limb pain, compressive neuropathy, pelvic pain, and spinal cord injury; 3) Vascular pain including chronic refractory angina, heart failure, ischemic pain due to peripheral vascular disease, and Raynaud’s syndrome.
The improvement provided by SCS may be very variable depending on the therapy and the source of pain. Chronic low back pain is one of the main indications for device implantation. We can differentiate these patients in two groups based on whether or not they have previous spinal surgery. Treatment with SCS has shown to improve pain in both groups by 48-55% (8), reaching up to 80% (8,9) with high frequency therapy. Other entities, such as CRPS, experience an improvement of more than 50% in 73% of patients undergoing SCS (10). With regard to the treatment of vascular pathology (both peripheral and anginal), studies show an improvement of more than 50% of pain in 85-88% of patients, in addition to an increase in blood flow and a decrease in amputations (11).
The aim of our study is to analyze the diagnostic indications of SCS therapy during the last 5 years in our hospital, to know what are the most common causes of pain for the indication of the implant of the device, as well as studying the relationship with sex and age. In addition, secondary objectives of the study are to analyze the improvement described by patients after implantation of the neurostimulator and to describe the relationship it has with the other variables.
MATERIAL AND METHODS
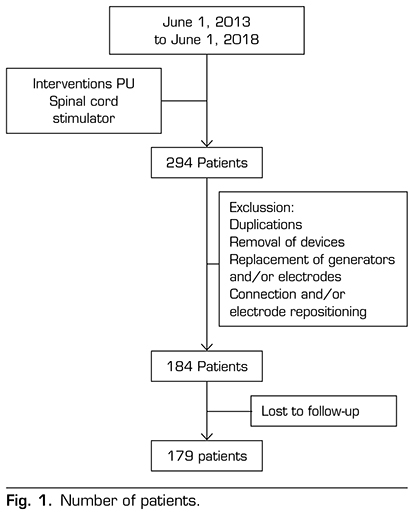
This is an observational, descriptive and retrospective study. Patients were identified from the surgical activity record of the Pain Unit of the General Hospital of Valencia. The study was approved by the hospital ethics committee. Patients who underwent definitive spinal cord stimulator implant surgery were included. After a first time, patients underwent a test period with an external generator. The indication of the definitive implant was based on an improvement greater than or equal to 50 %. The inclusion period was from June 1, 2013 to June 1, 2018. A total of 294 patients were identified. Duplications for 2 times of surgery, device removal, generator and/or electrode replacements, and connection and/or electrode repositioning were excluded from the analysis. Then, five patients were lost to follow-up, so they were excluded too. The final number of patients included was 179 (Figure 1). A database was set up including as variables the intervention performed, date of intervention, sex and age of the patient, improvement described by the patient expressed as a percentage at 6 months after the device was implanted, and diagnostic indication for SCS. The diagnoses were divided into groups: Failed back surgery syndrome (FBSS), complex regional pain syndrome (CRPS), low back pain without previous spinal surgery or “virgin back” (which includes facet syndrome, low back pain or spinal canal stenosis), neuralgia/neuropathic pain, ulcers, pelvic pain, headache, vasculopathy, cervical pain, and others. The group “other” includes diagnoses with an incidence of less than 1% (hemiplegia, phantom limb syndrome, non-revascularizable angina, and Raynaud’s disease).
We performed the descriptive statistics of the clinical epidemiological variables. For qualitative variables, absolute frequencies (expressed in numbers) and relative frequencies (expressed in percentages) were calculated over the total of cases and for quantitative variables their mean values and standard deviations were described. The Pearson correlation index was used for the analysis of the differences between quantitative variables. The Student’s t test was performed to analyze differences between quantitative variables and qualitative variables. A P value below 0.05 was considered statistically significant difference.
RESULTS
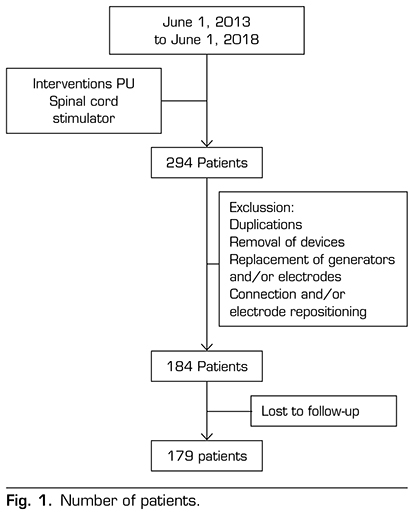
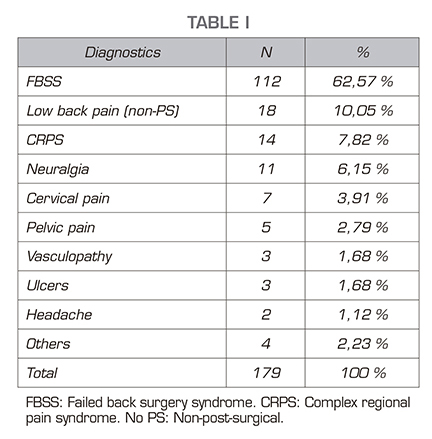
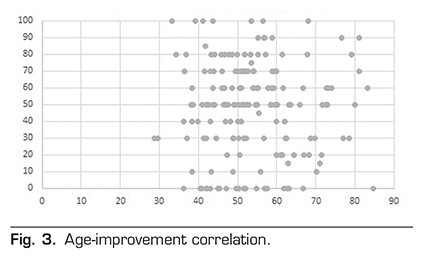
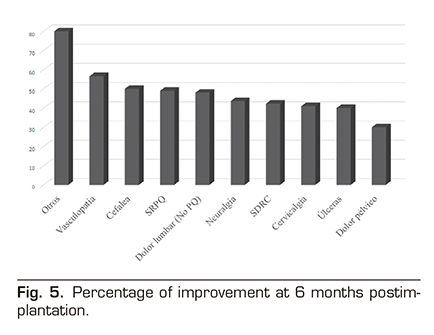
Table 1 shows the diagnoses for the indication of neurostimulator implant. FBSS was the diagnostic indication in 112 patients (62.57 %). Lumbar pain without previous spinal surgery was the diagnostic indication in 18 patients (10.05 %). CRPS was the diagnostic indication in 14 patients (7.82 %). Neuralgia or neuropathic pain was the diagnostic indication in 11 patients (6.15 %). Cervical pain was the diagnostic indication in 7 patients (3.91 %). Pelvic pain was the diagnostic indication in 5 patients (2.79 %). Peripheral vascular disease was the diagnostic indication in 3 patients (1.68 %). Ulcer pain was the diagnostic indication in 3 patients (1.68 %). Headache was the diagnostic indication in 2 patients (1.12 %). Other diagnoses involved the indication in 4 patients (2.23 %). A total of 55.86 % were women (100 patients), whereas 44.14 % were men (79 patients). The mean age of patients undergoing neurostimulator implantation was 53.6 ± 11 years. Figure 2 shows the age distribution by year. The mean age of FBSS patients in the sample was 53.37 years, similar to that of the group with other diagnoses that was 53.65 years. The mean percentage of improvement reported by patients was 47.99 ± 27.3 % at 6 months after implantation of the SCS. The percentage of improvement is not determined by the age of the patients, finding a Pearson correlation index of -0.014 (Figure 3). No differences in improvement have been found between sexes (Figure 4), the mean was 46.9 ± 28 % and 49.3 ± 26.4 % for women and men, respectively.
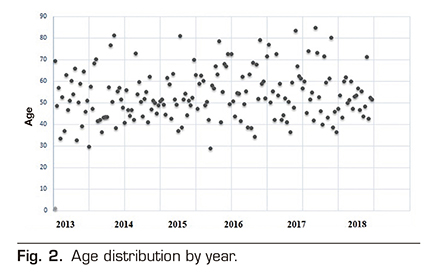
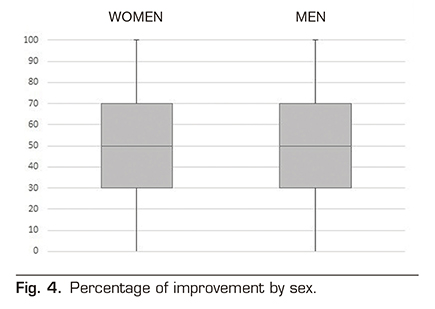
Student t test 0.57 (P value 0.568). No differences were found in the improvement according to the diagnostic indication, being 49.02 ± 25.89 % for the FBSS and 46.23 ± 29.71 % for other indications, with a P value of 0.514.
DISCUSSION
Neurostimulation of the spinal cord is a therapy for the treatment of chronic pain with high evidence (6) that, together with the favorable results shown in long-term cost-effectiveness analysis (5,6), makes it an indicated treatment in many situations. In our study we have found up to 15 different diagnostic indications for the implantation of this device. In spite of the variability of diagnoses in which this therapy may be indicated, it is notably that in more than half of the cases (62 %) the indication is FBSS. The incidence of this entity after spinal surgery is 5-40% and the efficacy of neurostimulation in pain control was demonstrated (8,9,12). No age-related variability was found in the diagnosis or the disease progression over time. The mean improvement rate was close to 50 % (47.99 %). This variable expressed in percentage is of high clinical value. Despite the use of a numerical scale would be more appropriate in research, the percentage of improvement or the overall impression of change by patients have shown to be well related to the numerical scales in the treatment of chronic pain (13,14,15). In our study, age and sex showed no influence on patient improvement. Figure 5 shows improvement in each diagnostic indication. This improvement presents a significant variability depending on the diagnosis indication of the implant, without significant differences between the majority indication and the rest. Vascular disease (either coronary or peripheral) is one of the indications that showed a higher rate of improvement, as has already been shown in several studies (6,16,17). However, despite the evidence in this regard, the low number of patients referred from these services to our unit to consider SCS therapy is noteworthy. The improvement in patients with chronic low back pain (whether they had previous surgery or not) was around 50%, consistent with the improvement reported in other studies (8,9). However, if we analyzed the etiology of lumbar pain by subgroup, attention is drawn to the low percentage of improvement in patients with facet syndrome (27.5 %) compared to the other patients with lumbar pain (53.88 %). It is estimated that the facet syndrome accounts for 27-40% of chronic low back pain (18). Many therapies showing effectiveness in treating this syndrome are available; however, we have found no significant improvement in patients after a neurostimulator implant.
Although several studies (16) show higher rates of improvement than ours, it should be considered that many factors influence (analgesic treatment, psychological condition, type of therapy) that have not been analyzed in this study, and this might be a limitation of this study.
REFERENCES