DOI: 10.20986/resed.2018.3695/2018
REVISIÓN
Dexmedetomidine as an adjuvant to peripheral nerve block
A. Rojas González
Servicio Anestesia y Pabellón. Unidad de Dolor Agudo. Hospital Puerto Montt. Facultad de Medicina. Universidad San Sebastián. Puerto Montt. Chile
Received: 27-06-2018
Accepted: 28-06-2018
Correspondence: Andrés Rojas González
andresirijillo@gmail.com
ABSTRACT
Introduction: Dexmedetomidine (DEX) is a multifunction drug proposed in recent years as an adjuvant for regional nerve blocks with local anesthetic (LA).
Objetives: to evaluate the analgesic properties of this α-2 agonist when added to LA in different peripheral nerve block approaches (regional anesthesia), in terms of the quality of the analgesia obtained and potential associated complications.
Materials and methods: Narrative review, using MeSH terms (English-Spanish), widely-known search engines, considering the last 5 years to date (among other filters), analyzing systematic reviews, meta-analysis or clinical trials comparing nerve blocks with/without perineural DEX added to long-term LA.
Results: In general terms, it’s observed with this selective α-2 agonist, that the blockade latency decreases -19.16 %, increases analgesia duration + 60,79 % and motor blockade + 54,71 %; decreasing postoperative opioids – 49,54 % and LA consumption – 52,00 %, which would be explained by an intrinsic mechanism at perineural level. Its association with cardiovascular depression and sedation (both transient, reversible and without major clinical consequences) is dose-dependent, recommending 0,5-1 μg/kg perineural (maximum 100 μg).
Conclusions: In terms of risk-benefit, perineural DEX improves the quality of analgesia obtained with minimal associated adverse effects.
Key words: Dexmedetomidine, anesthetics, local analgesia, anesthesia, nerve block.
RESUMEN
Introducción: Dexmedetomidina (DEX) es un fármaco multifunción propuesto en los últimos años como coadyuvante para bloqueos regionales con anestésico local (AL). Objetivos: Evaluar las propiedades analgésicas de este α-2 agonista al adicionarse a AL en diferentes abordajes de bloqueo de nervio periférico (anestesia regional), en términos de calidad de la analgesia obtenida y potenciales complicaciones asociadas.
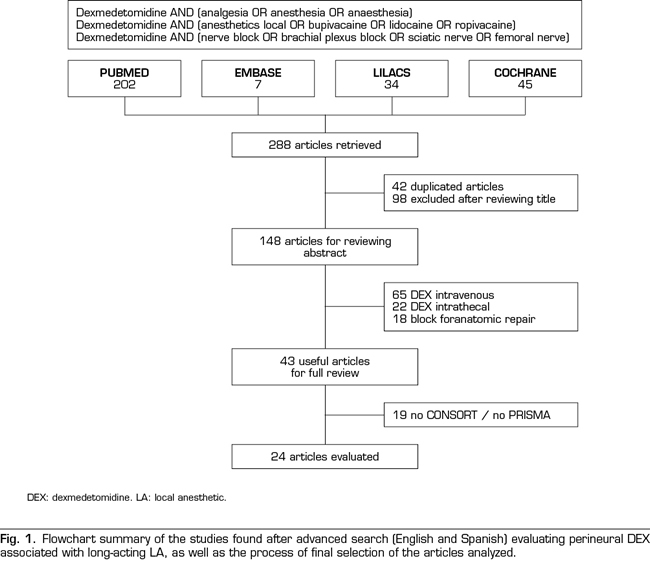
Materiales y métodos: Se llevó a cabo una revisión narrativa, utilizando términos MeSH (inglés-español), con motores de búsqueda ampliamente conocidos (PUBMED, EMBASE, COCHRANE y LILACS), considerando los últimos 5 años a la fecha (entre otros filtros), analizando revisiones sistemáticas, metanálisis o ensayos clínicos que comparasen bloqueos regionales con AL de larga duración con/sin DEX perineural.
Resultados: En líneas generales, al utilizar este α-2 agonista selectivo, la latencia del bloqueo disminuyó – 19,16 %, aumentó la duración de la analgesia + 60,79 %
y bloqueo motor + 54,71 %; reduciendo además consumo de opioides – 49,54 % y anestésicos locales – 52,00%, lo cual se explicaría por un mecanismo de acción intrínseco a nivel perineural. Su asociación a depresión cardiovascular y sedación (ambas transitorias, reversibles y sin mayor repercusión clínica) es dosis-dependiente, recomendándose 0,5-1 µg/kg perineural (máximo 100 µg).
Conclusiones: En términos de riesgo-beneficio, DEX perineural mejora la calidad de la analgesia obtenida con mínimos efectos adversos asociados.
Palabras clave: Dexmedetomidina, anestésicos, locales analgesia, anestesia, bloqueo nervio.
INTRODUCTION
The first α-2 agonist synthesized in the early 1960s was clonidine, introduced to the pharmaceutical market as a nasal decongestant. However, in 1966 it was re-cataloged as antihypertensive due to the predominance of its sedative and cardiovascular depressant side effects.
Given the above, it was incorporated into the therapeutic arsenal of the Critical Care Unit (CCU) and Medicine, but over the years, and due to its potential analgesic properties, it became a tool for the anesthesiological management of certain patients, performing to date a role (somewhat limited) in the control of pain, improvement of hemodynamic and sympathetic stability, as well as reduction of postoperative nausea and vomiting (PONV) (1).
About 30 years later, and in 1999, after approval by the Food and Drug Administration (FDA) of the United States, a new and more selective α-2 receptor agonist, dexmedetomidine (DEX), was introduced mainly for sedation/short-acting analgesia of patients on mechanical ventilation (2).
Over the years, the use of DEX was extrapolated to the perioperative period, mainly as premedication, auxiliary anesthetic for awake intubation and procedural sedation and analgesia, especially for those patients with high risk of postoperative delirium. In 2004, and after understanding a little more its mechanism of action, the first studies of DEX as adjuvant of local anesthetics (AL) in regional blocks were conducted, this with the ultimate goal of improving the quality and duration of analgesia obtained (3).
The problem of peripheral nerve blocks, which are commonly used as analgesia (and even anesthesia) especially in limb surgeries, is that if they are not used in association with a continuous infusion catheter, they would provide a relatively short duration of effect (4). Therefore, in the search to extend the duration of single-dose blockade, multiple adjuvants have been studied, confirming so far only the advantages of the use of epinephrine and dexamethasone in this area, increasing the duration of analgesia by 20-30%, specially in brachial plexus blocks, whereas other drugs, such as benzodiazepines, anti-inflammatory drugs or clonidine, have not been able to demonstrate their real effectiveness when added to AL in peripheral nerve blocks (5-7).
Therefore, and knowing the potential analgesic benefit of the DEX, in the last 5-10 years various clinical trials have studied the effectiveness of DEX as a perineural adjuvant in regional anesthesia, obtaining promising results so far (8).
The objective of this study is then, in a complementary way of systematic reviews and meta-analyzes that have studied the role of DEX in brachial plexus blocks, to evaluate the analgesic properties of this α-2 agonist when added to the treatment with LA but in different approaches for regional anesthesia, this because we believe the analgesic role of DEX is independent of the type of peripheral nerve block used.
Accordingly, the results of the publications found were critically analyzed, emphasizing the quality of the analgesia obtained (and potential adverse effects) and comparing peripheral nerve blocks with DEX versus without DEX as a long-acting adjuvant of AL.
We declare that the present investigation has not received any specific grant from agencies of the public or commercial sectors, and it was developed not-for-profit.
METHODOLOGY
A narrative-type review to know the effectiveness, in terms of the quality of the analgesia obtained, of peripheral nerve blocks with long-acting LA and the addition or not of DEX as an adjuvant in regional anesthesia-analgesia. Despite not being a systematic review (because the performance of this α-2 agonist was assessed in different contexts and not one in particular), PRISMA recommendations were followed to keep an order and transparency in the presentation of the data obtained and analyzed.
Literature search
The search engines PUBMED, EMBASE, COCHRANE and LILACS were used. Cross-search strategy using free terms and Medical Subject Headings (MeSH terms) and their respective translation into Spanish (dexmedetomidine; analgesia; anesthesia; nerve block; brachial plexus block; sciatic nerve; femoral nerve; anesthetics, local; bupivacaine ; lidocaine; ropivacaine), Boolean operators (AND, OR and NOT) and review of references recommended by the same publications cited were used.
Selection criteria
The criteria used to define the studies included for analysis were: systematic review (SR), meta-analysis (MA) and randomized clinical trials (RCT) in regional anesthesia, comparing the addition of perineural DEX to long-acting LA (bupivacaine, levobupivacaine or ropivacaine) versus only AL long-acting without DEX or other adjuvant, in any type of peripheral nerve block, with execution of the block by ultrasound and/or nerve stimulation (excluding anatomical reference for higher failure rate). Studies that only used perineural DEX or in which DEX was administered by another route were excluded. Bier’s block was also not considered. The selected studies had to adhere to PRISMA initiative if they were SR/MA and to CONSORT initiative if they were RCT. Patients had to be over 18 years of age, any sex, year of publication of the study from 2012 to date (last 5 years), in English or Spanish language, and without publication bias. Figure 1 summarizes all the articles found and the selection process used for those studies finally included for analysis.
Data collection
Given that it is a study conducted by a single author, it was decided to include the largest number of studies that met the inclusion criteria described, extracting the data of interest and then presenting them in the attached tables. Latency period of the blockade, duration of analgesia obtained up to the first requirement made by the patient and duration of the motor block were investigated for limb blocks. For central blocks, considering that most of them are continuous, opioid consumption was also evaluated. The information presented regarding adverse effects (hypotension, bradycardia and sedation) was obtained directly from the SR/MA because this information is already available.
PHARMACOLOGICAL PROPERTIES
Dexmedetomidine is the dextro enantiomer of medetomidine, a methylated derivative of detomidine, an imidazoline receptor agonist. It has affinity for receptors α-2: α-1 much more specific (1620:1) than its precursor clonidine (200:1), which is why it has less adverse effects than the latter (9).
The route of administration of DEX is mainly intravenous (i.v.). However, it can also be absorbed systemically through subcutaneous (s.c.), buccal or intramuscular (i.m.) routes, reporting a bioavailability of 104% for the latter. Its approximate latency is 15 minutes, reaching peak plasma in 60 minutes after continuous infusion at the dose suggested by the manufacturer (Precedex®, Abbott Labs) of 0.2-0.7 μg/kg/h, with an elimination half-life (t½ β) of 120-150 minutes (10).
The total elimination of DEX from plasma is independent of age; therefore similar doses of infusion can be used in children and adults. However, a higher risk of hypotension and bradycardia (dose-dependent) has been reported in subjects over 65 years of age, so a reduction in the dose is recommended for this population (11).
Furthermore, its duration is directly related to its binding capacity to albumin and glycoprotein α-1, which remains constant despite the various concentrations of the drug. Therefore, the binding fraction decreases and the free fraction increases in patients with hepatic dysfunction or severe malnutrition, so the dose must also be reduced in these patients (12).
The metabolism of DEX occurs in the liver through cytochrome P450, there are no known active or toxic metabolites (which are eliminated by 95% in urine), and can be used safely in patients with renal failure (13).
In addition, the effect of DEX can be reversed in a dose-dependent manner with the selective α-2 antagonist atipamezole. However, this drug is not approved for use in humans, and therefore, it is usually available in the pharmacological armamentarium of veterinarians (14).
MECHANISM OF ACTION IN REGIONAL ANESTHESIA
Many available writings explain in detail the functioning of DEX. The α-2 adrenergic receptor consists of three α-2 isoreceptors (α-2a, α-2b and α-2c), which regulate the various pharmacodynamic effects of this drug (15). The α-2a receptor seems to promote sedation and anxiolysis in the locus coeruleus, as well as to generate bradycardia and peripheral vasodilation by stimulation of the cerebral vasomotor center. The α-2b receptor prevents tremor, generates analgesia in the dorsal horns of the spinal cord and determines peripheral vasoconstriction. The α-2c receptor modulates the mental state.
At the second messenger level, and once any of these adrenoreceptors are activated by DEX, adenylate cyclase is inhibited, the production of cyclic adenosine monophosphate (cAMP) decreases, and noradrenergic neurons (mainly presynaptic neurons) are hyperpolarized by the potassium exit and calcium entry block in the terminals of the neurons.
This change in the conductance of the ions inhibits the stimulation of the locus coeruleus, dorsal horns and extraspinal localizations, thus decreasing the discharge of the nociceptive fibers Aδ and C and ultimately generating the desired analgesic effect (16).
In relation to these extra-spinal localizations of α-2 receptors, the interest of the study of DEX as an adjuvant drug in regional anesthesia arises.
Using perineural 0.5% ropivacaine plus DEX (20 μg/kg), Brummett et al. reported an extension of the sensory and motor block of the sciatic nerve in rats from 120 to 210 minutes compared to 0.5% ropivacaine and physiological saline solution (PSS) or 0.5% ropivacaine with subcutaneous DEX (p <0.001), also evidencing lower associated systemic effects (17).
Knowing then the analgesic benefits of DEX, some authors have argued that regardless of its administration route (perineural versus i.v.), and due to its central mechanism of action, the opioid consumption will decrease and the duration of the sensory block will be prolonged, however, there are only 2 studies in this regard that support these postulates (18,19,20).
More recently, studies conducted in rats with direct nervous exposure to various combinations of drugs (including DEX and ropivacaine) have shown that the instillation of antagonists α-1 (prazosin) and α-2 (idazoxan) does not alter latency or duration of sensorimotor block obtained with DEX. However, the direct application of forskolin, an agonist of cyclic nucleotide-gated ion channels (Ih), in the nerve attenuated, in a dose-dependent manner, the sensorimotor blocking effect when used the combination of ropivacaine and DEX. This effect was not attenuated when ropivacaine with PSS was used. The authors posed that agonism in these Ih receptors would activate adenylate cyclase, increasing cAMP levels in the nerve and avoiding nervous hyperpolarization, the substrate of functioning of the α-2 agonists (21,22).
DEXMEDETOMIDINE AND UPPER LIMB BLOCKS
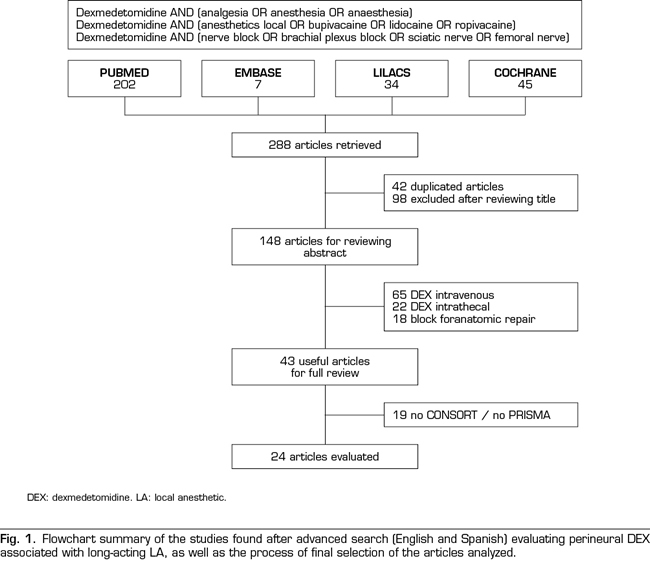
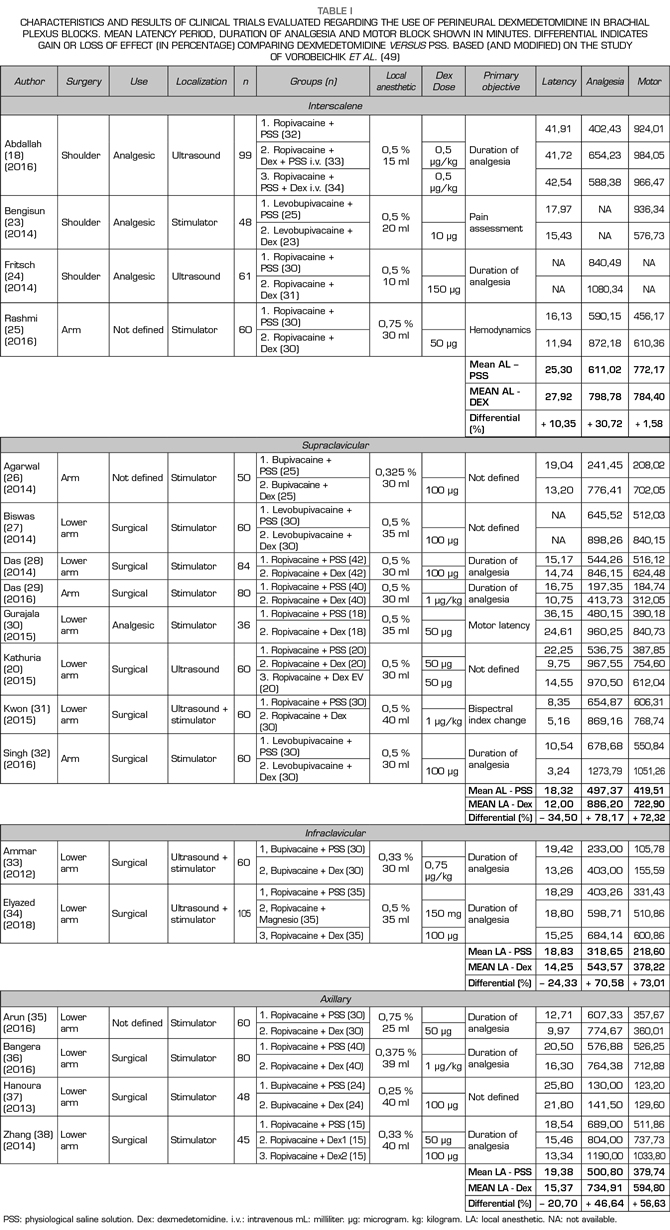
Table I summarizes the results of interest in relation to the primary objective of this study in the subgroup of regional anesthesia for upper extremity. First, it should be noted that all the articles analyzed correspond to RCT comparing results of peripheral nerve blocks with and without the use of perineural DEX in different brachial plexus approaches. In general terms, the analyzed studies are very heterogeneous regarding surgical context and anesthetic methodology, even so, most of them present a moderate-high level in terms of quality of evidence (according to GRADE scale) and a moderate-low level of bias (according to the COCHRANE scale) (18,20,23-38).
Important factors to consider prior to the interpretation of the results obtained are the variability of the AL (bupivacaine, levobupivacaine or ropivacaine) and the concentration and volume used (0.25-0.75%, 15-40 mL)
because the association between these factors and the block quality, especially motor, is known.
As indicated in the methodology, those trials where blockade was performed by anatomical reference were not considered. However, we should also consider potential biases when comparing the success rate of blocks performed using neurostimulation and/or ultrasound, impressing today as gold standard the use of ultrasound. Nevertheless, only 6 authors used ultrasound for the procedure (performed by experienced physicians as explicitly indicated) in our results and only 2 of them it was complemented with neurostimulation. The rest of the studies confirmed the blockade by obtaining an expected motor response with a stimulus ≤ 0.5 mA. It should also be noted that over 80% of these studies were performed in patients aged 18-65 years, American Society of Anesthesiologists (ASA) I-II, in the context of open or arthroscopic upper extremity trauma surgery (with an evident painful component associated).
In objective terms, we observed that when using perineural DEX (in dosing 0.5-1 μg/kg with maximum 100 μg), without other adjuvant, in brachial plexus blocks with long-acting LA (and regardless of the type of approach), the block latency was reduced by an average of 15.11% (20.45 to 17.38 minutes), the duration of the analgesia increased by an average of 53.76% (481.81 to 740.86 minutes) and the duration of motor block increased by an average of 38.56% (447.50 to 620.08 minutes) (18.20.23-38).
DEXMEDETOMIDINE AND LOWER LIMBS BLOCKS
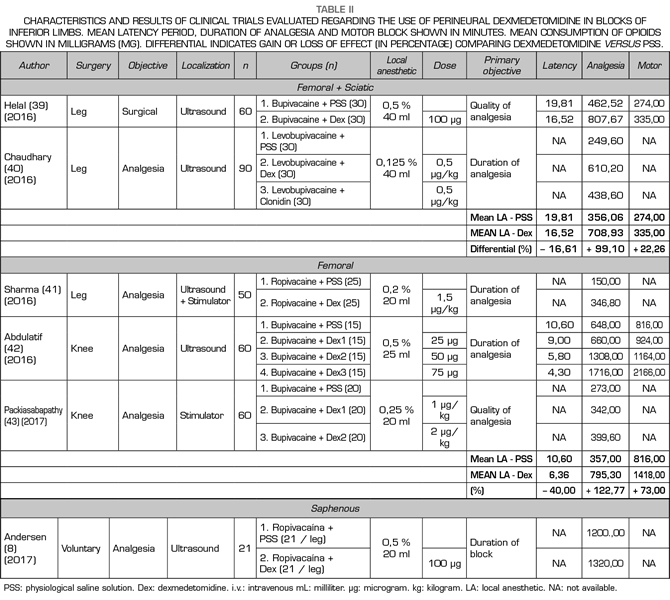
Similarly to the clinical trials that investigated the performance of perineural DEX in the upper extremity, most of the studies analyzed in this section had a moderate level in terms of quality of evidence (GRADE) and bias (COCHRANE). All the studies analyzed in this subgroup were performed in patients aged over 18 years, ASA I-II and with the aim of undergoing analgesia for trauma surgery of the knee or ankle (Table II) (8,39-43).
In this section it is difficult to establish a direct relationship between the dose of the perineural DEX and the duration of the analgesia after the blockade, because concomitant neuroaxial or general anesthesia was used in 4 of the analyzed studies. Concentration and volume of AL used subsequently was very varied (0.125-0.5%, 20-40 mL). In addition, a catheter was passed in some of the tests for continuous blockade of peripheral nerve, making even more difficult to establish a very accurate correlation between the perineural DEX and the first analgesia requirement requested by the patient (8,39-43).
In objective terms, we observed that when using perineural DEX (0.5-2 μg/kg), with long-acting LA, without other adjuvant, in lower limb blocks (femoral, sciatic and/or saphenous nerve), the latency of the blockade was reduced by an average of 41.42% (15.20 to 8.90 minutes), the duration of analgesia increased by an average of 67.84% (487.18 to 834.47 minutes) and the duration of the motor block increased by an average of 107% (545.00 to 1132.25 minutes). However, we must keep in mind when interpreting these results, especially with regard to motor block, that initially spinal anesthesia and/or continuous block catheter was used in several of the analyzed studies (40-43).
DEXMEDETOMIDINE AND CENTRAL BLOCKS
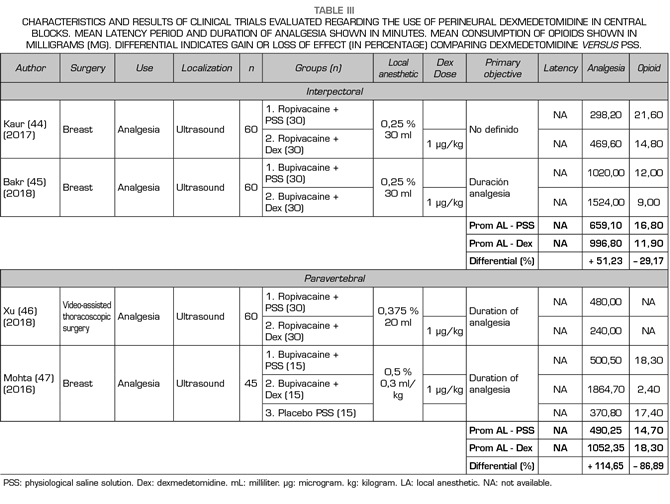
There is very little information available regarding the performance of perineural DEX added to AL in central trunk blocks, not finding to date, and based on the methodology used, more than 10-12 clinical trials in this regard. Table III summarizes the studies found based on the established methodological criteria
(44-47). Most of the trials evaluated are of a moderate level of evidence quality (GRADE) and bias (COCHRANE), were performed mostly in adult women, ASA I-II, and mainly in the context of oncological mastectomy (only Xu et al. studied DEX results in continuous paravertebral block for videothoracoscopy) (46).
Given that most clinical trials involved the use of general anesthesia and passing a catheter for continuous peripheral nerve block, latency periods could not be adequately studied and, therefore, this point was not evaluated in this subgroup. Considering the antecedents previously exposed, we found that when perineural DEX (1 μg/kg) was used with long-lasting LA (0.25-0.5%, 20-30 mL) , without other adjuvant, in interpectoral or paravertebral blocks, the duration of analgesia increased by an average of 78.28% (574.67 to 1024.57 minutes), no motor commitment was analyzed because these are essentially sensory blocks. Rescue opioid consumption was evaluated, finding an average reduction of 49.57% (17.30 mg of average morphine consumption in the first 24 hours with LA versus 8.73 mg morphine when adding DEX to nerve block with AL).
ADVERSE EFFECTS
The local toxicity of the perineural DEX has been investigated in animal models, demonstrating that both myelin and axon are not affected after this α-2 agonist is administered in a controlled and direct manner at high doses (20 μg/kg evaluated on days 1 and 14) (17,48,49). Clinically, paresthesias for up to 72 hours have been described in the innervation area. This occurred in 2 volunteers who received 150 μg of perineural DEX plus 3 mL of 0.75% ropivacaine in the ulnar nerve at the elbow (non-dominant arm and applied using ultrasound) (48).
Regarding other adverse effects, the risk of cardiovascular depression and sedation has been directly evaluated in most of the presented trials. All the authors reported that, if present, these complications have been transient and reversible, without major clinical consequences and, therefore, not requiring more therapeutic intervention (18,20,22-47).
According to the systematic review conducted by Vorobeichik et al., on the use of perineural DEX in brachial plexus blocks, the risk of associated complications increases exponentially in a dose-dependent manner (especially > 50 μg), with an odds ratio (OR) of 3.3 times for bradycardia (p <0.01), 5.4 times for hypotension (p <0.01) and 17.2 times for sedation (p <0.01), when compared to blocks only treated with LA. In this regard, we must point out the non-standardization in the scale used for the measurement of sedation, even so, no associated hypoxic events were reported (49). Finally, the risk of PONV was low and similar in patients with blocks with and without perineural DEX (49).
CONCLUSIONS
Out of the multiple adjuvants used in regional anesthesia, and after analyzing multiple and diverse studies, perineural DEX seems to improve the quality of the analgesia obtained based on peripheral nerve blocks.
Even if the optimal dose of this α-2 agonist is unknown in this context, a dose of 0.5-1 μg/kg perineural with a maximum limit of 50-100 μg is impressive enough in terms of risk-benefit according to the literature analyzed.
Regarding the advantages of DEX, we found that globally (the sum effect of the different types of blocks analyzed), when adding DEX to long-acting LA for regional anesthesia, the latency of the blockade decreases (-19.16%), the duration of analgesia increases
(+ 60.79%), increases the duration of motor blockade (+ 54.71%) and decreases opioid consumption (-49.54%).
Among its disadvantages, the hemodynamic changes and associated sedation are dose-dependent, transient and without major clinical consequences (in selected populations) and they are of minimal incidence using the dose indicated above (19,49).
It is impressive then that the benefits of perineural DEX outweigh its risks. However we must keep in mind that, despite being a well-known medication, regularly used in CCU and wards, its application in regional analgesia is not yet approved in Spain and other countries, therefore future multicenter trials are needed to allow their approval in this area by the relevant regulatory bodies of each country.
Then, the decision of using this α-2 agonist in regional anesthesia will depend on the criteria of the treating anesthesiologist, always prioritizing the principle of beneficence and non-maleficence, especially in populations with high cardiovascular risk, sleep apnea syndrome, potential difficult airway and outpatient surgery, whose recovery and hospital discharge could be hindered by the increase in motor blockade (increased risk of falls).
Therefore, corresponds to the future to investigate in more detail the best dose of this drug, to see if it is globally authorized for its application at the perineural level, to define whether or not the administration route alters its clinical effect and if it is modified with the addition of other adjuvants. Even so, and based on the information presented, we believe that perineural DEX should be considered as part of the pharmacological arsenal commonly used in regional anesthesia and postoperative pain control.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
BIBLIOGRAPHY